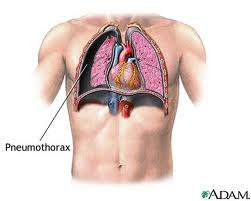
Hemothorax patient death can be caused because of the large blood loss and the occurrence of respiratory failure.
Respiratory failure due to the large amount of blood in the pleural cavity pressure of lung tissue and reduced lung tissue that does ventilation.

Then treatment hemothorax as follows:
1. Emptying of blood from the pleural cavity.
Tags : Management Hemothorax, Hemothorax procedure, Thoracotomy, hemothorax treatment, haemothorax, hemothorax
Respiratory failure due to the large amount of blood in the pleural cavity pressure of lung tissue and reduced lung tissue that does ventilation.

Then treatment hemothorax as follows:
1. Emptying of blood from the pleural cavity.
Installed "chest tube" and is connected with the WSD system, this can accelerate the lung expands.2. Stop the bleeding.
3. General state of repair.
If the installation of WSD, the blood still does not stop, then considered for thoracotomy.
Giving oxygen 2-4 liters / minute, the length adjusted to the clinical changes, better yet, if the monitored with blood gas analysis. Try to people with normal blood gases.4. Others.
Giving blood transfusion: seen from a decrease in Hb.
As a benchmark can be used the following calculation, every 250 cc of blood (from patients with Hb 15 g%) can raise ¾ g% Hb.
Given with a normal drop of about 20-30 drops / minute and maintained not to an interruption in heart function or cause interference with the heart.
- Antibiotics, carried out if there is secondary infection.
Antibiotics are used adjusted to the sensitivity test and culture. If the infecting organism is unclear, while the state of serious illnesses, then the patient can be given a "broad spectrum antibiotic", for example, ampicillin at a dose of 4 x 250 mg daily.
Also considered in case of pleural thickening decortication.
Tags : Management Hemothorax, Hemothorax procedure, Thoracotomy, hemothorax treatment, haemothorax, hemothorax